In a first of its kind in New Zealand, a cultivation licence has been granted for research into an indigenous magic mushroom that is hoped to be able to help those suffering from methamphetamine addiction. The Ministry of Health granted the licence for Psilocybe Weraroa, a variety of mushroom that contains psilocybin, the active ingredient in magic mushroomsPsilocybin is an illegal Class A substance under the Misuse of Drugs Act, but the Director-General of Health can grant licences for research or medicinal purposes.
The licence is held by Rua Bioscience, a biopharmaceutical company based in Tairāwhiti, and is a crucial piece of the puzzle in a collaboration with a long-term goal of helping whānau affected by methamphetamine and other addictions.
Rangiwaho Marae – also based in Tairāwhiti – is planning clinical trials with Psilocybe Weraroa, with the support of a network involving rongoā Māori practitioners, Environmental Science and Research (ESR), Auckland and Waikato universities, Manaaki Whenua Landcare Research, Mātai Medical Research Institute, an iwi health provider and other community stakeholders.
“We are hugely excited about this opportunity for our whānau” said Rangiwaho trustee Jody Toroa.
“These taonga are provided by the atua and our people have been using them for healing and wellness for centuries. We have been learning from tohunga (expert practitioners) about how the taonga can help shift ingrained habits and unhelpful ways of thinking, to open up new possibilities.”
Rua Bioscience chief executive Paul Naske described it as a ground-breaking project into “potentially life-changing medical research”.
“Collaborating with Rangiwaho, ESR, rongoā practitioners and university medical researchers provides us with a unique opportunity to explore cultivation techniques that can contribute to research undertaken in a culturally safe environment.
“Bringing together Mātauranga Māori, psychedelic traditions and contemporary neuroscience research is world-leading innovation based here in Tairāwhiti. We are excited to be able to support this kaupapa.”
The New Zealand East Coast is a problem area for methamphetamine use. The latest ESR wastewater survey shows the highest per-capita methamphetamine consumption in Northland, followed by Waikato and then the East Coast region.
The Labour Party’s 2020 election manifesto promised to roll out the highly-lauded meth-treatment programme Te Ara Oranga to the East Coast and the Eastern Bay of Plenty, but the Labour Government only delivered in the latter region.
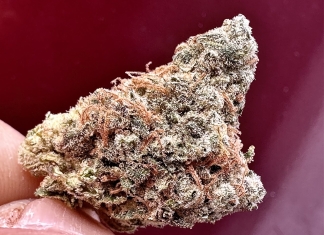
Mushroom therapy
The licence is only for cultivation research at this stage, and clinical trials would require further Medsafe approval.
The first trial would be into healthy adults to test the safety profile. No substance is zero risk, but the scientific community considers psilocybin to be less harmful than most other illegal drugs including amphetamines, opioids and cannabis, while legal substances alcohol and tobacco usually top the list of the most harmful.
Psychdelics such as psilocybin and LSD are thought to increase neural plasticity. A brain that’s more changeable, with different networks talking to each other more, might more easily free someone from deeply entrenched and habitual ways of thinking – such as the kind of rumination trough that can lead to depression.
A team at the New Zealand University of Auckland is at the stage 2 phase of clinical trials into microdosing LSD for depression. This followed earlier findings where those who had microdosed LSD for a period of six weeks reported improved mood, less irritability, and increased energy, creativity and connectedness, with minimal safety issues.
Psilocybin has been the subject of clinical trials around the world looking into potential therapeutic benefits for a range of issues such as opioid addiction, Alzheimer’s disease, post-traumatic stress disorder (PTSD), eating disorders, and alcohol use in people with major depression.
It is part of a resurgence in medical interest in psychedelic substances that started in the 1950s, but came to a screeching halt with the moral panic that saw them made illegal in the late 1960s and early 1970s.
There has since been a revival, with Australia leading the way. Psychiatrists there can prescribe MDMA (also known as party drug Ecstasy) for post-traumatic stress disorder and psilocybin for some types of treatment-resistant depression.
Last year the Australian Government gave more than $16 million to support seven clinical trials into the potential efficacy of treating mental health issues with psilocybin, MDMA, DMT, and CBD.
The Government in New Zealand has not shown any appetite at this stage to support such treatment, though the Health Research Council has independently supported different research projects into psychedelics, including this one.
The council has granted $300,000 over 18 months to Rangiwaho Marae for its clinical research programme.
“Their aspirations for this mahi is to comprehensively investigate the therapeutic potential of natural psychoactive molecules derived from taonga species in collaboration with iwi communities and Māori businesses,” said the council of the grant, “and to develop tikanga Māori (protocol) for safe administration of psilocybin-containing taonga species of mushroom (Weraroa) for the treatment of addiction and other mental health conditions such as depression in a marae setting, by, with and for Māori.”
First for New Zealand
No one in New Zealand has been prescribed psilocybin to date in a clinical setting. Three applications have been made for using psilocybin in clinical trials, all in the past 18 months.
It’s unclear at this stage what kind of psilocybin dosage – a full dose or a microdose, or something in between – would be involved in the Rangiwaho clinical trials.
A goal of the cultivation phase – with ESR providing analytical testing services – is to determine the levels of psilocybin in the fungi and the consistency of these levels. This would help ensure accurate dosing in human trials.
Set and setting have proven vital in the effectiveness of a full dose of psilocybin, and the Rangiwaho trials are being planned with an emphasis on the therapeutic process as well as the substance.
A number of rongoā practitioners are involved in the development of the clinical research programme and will participate in the clinical trials, providing guidance and support to participants.
A local GP and nurse are involved in the research design and planning, and medical doctors and health researchers from the School of Medicine at the University of Auckland and the University of Waikato have been supporting the research.
A medical doctor would be involved in prescribing during the clinical trials, including the pre-screening and post-session follow-up consultations.
Psilocybe Weraroa is one of seven varieties of magic mushroom endemic to Aotearoa. The initial licence allows for one variety, but the project team hopes to add more species in the future.
Naske emphasised that this development would add to the botanical pharmaceutical focus of Rua Bioscience, was cost-neutral, and in no way detracted from the commercial priorities of the company which is currently selling cannabis-derived medicines in Europe and Australia.